Welcome to the Research and Strategy Services at in today's fast-paced.


The findings of a recent research study found that the parasympathetic nervous system restrains breathing and slows the heart rate of sleeping children that suffer from epilepsy substantially more than that of what is modulated in healthy children. Findings of this nature could have major implications in diagnosing and treating epilepsy, as well as in understanding sudden unexpected death in epilepsy.
Until now, epilepsy has been characterized by doctors as a brain disorder. However, thanks to this study, researchers at Case Western Reserve University have found evidence that part of the autonomic nervous system functions in a different manner during the absence of a seizure. A connection of this sort, to the involuntary division of the nervous system, could have implications for treating and diagnosing the disease. Not only that but also in understanding sudden unexpected death in epilepsy (SUDEP).
Roberto Fernandez Galan, the assistant professor of electrical engineering and computer science and senior author of the study, stated “All of the findings of our study on heart rate variability in epilepsy point to increased activity in the parasympathetic nervous system during sleep.” He goes on to say, “But, we do not know if this abnormality compensates for epilepsy, coincides with the disease or is part of the etiology.” Specifically, he refers to the parasympathetic (or “rest and digest”) nervous system that modulates the breathing and slows the heart rate of children with epilepsy while they sleep significantly more than that of what takes place in healthy children.
To the researchers’ surprise, during the study, it was revealed that several children who had previously been diagnosed as neurologically normal – but that showed similar strong modulation as well as lower heart rates – were to be later diagnosed with epilepsy. This discovery offers suggestive evidence that changes in the parasympathetic tone precede the onset of epilepsy diagnosis in children.
In the study, the researchers examined the electrocardiograms of 91 adolescents and children who had been diagnosed with generalized epilepsy and 25 neurologically normal children. The subjects were observed during 30 minutes of stage 2, also referred to as light sleep. During the intervals care was taken to ensure that no patients were suffering from a seizure during the intervals.
During the study, the researchers found that an increase in the heart rate during inhalation and decrease during exhalation – or respiratory sinus arrhythmia –was more pronounced in the epilepsy patients, whose heart rate was significantly lower.
The changes proved to be consistent with the increased firing of the vagus nerve in children who had been diagnosed with epilepsy, as compared to those children who had not been diagnosed with epilepsy. The vagus nerve serves as the primary trunk of the parasympathetic nervous system. The more rapidly that the vagus nerve fires, the more it slows the heart, which is especially true during exhalation.
Galan claims that by further defining the differences in the respiratory arrhythmia between children who suffer from epilepsy and those who do not, they may have the ability to identify biomarkers, or thresholds, to diagnose those who have the disease or even those at increased risk for developing it. Furthermore, the researchers say that the findings also present the possibility that medications can help to control the autonomic nervous system which in turn may help to control epilepsy.
Research from this study is published in the online Journal of Neurophysiology.
(Source)




Welcome to the Research and Strategy Services at in today's fast-paced.

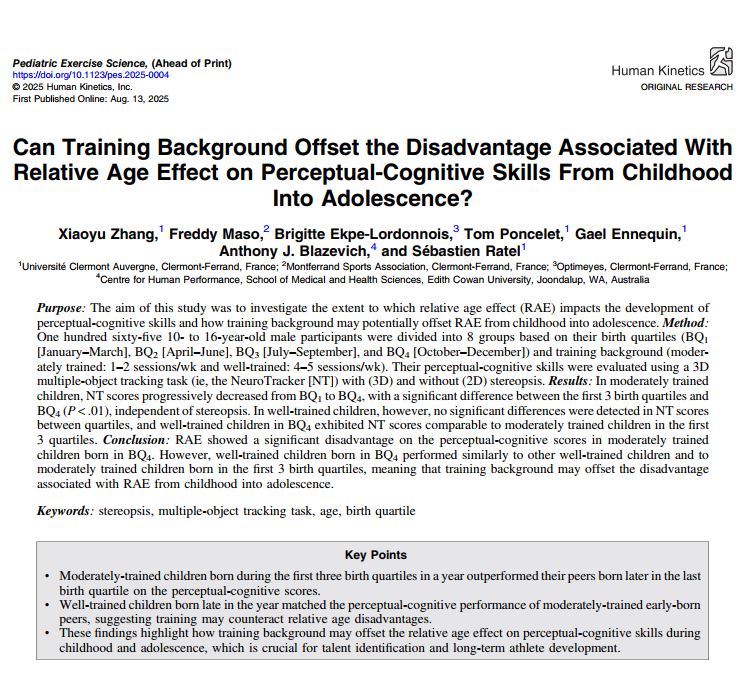
Many professional roles require cognitive performance to be sustained over long periods rather than demonstrated briefly. This article explains how sustained cognitive load shapes performance in knowledge-work and monitoring environments.

An overview of the important interpretational difference between temporary changes in brain state, and durably lasting changes in cognitive capacities.

An interpretive overview explaining why cognitive training outcomes vary across individuals, how factors such as baseline ability, state, and measurement influence results, and why variability should be expected.
.png)